Model name: Papillomavirus Rapid Interface for Modelling and Economics (PRIME)
Modellers: Mark Jit, Marc Brisson, Kaja Abbas, and Han Fu
Institution: London School of Hygiene & Tropical Medicine (LSHTM)
PRIME is a static model of HPV vaccination that uses proportional impact to estimate the cost-effectiveness of HPV vaccination in low- and middle-income countries. It was developed by LSHTM in collaboration with researchers from the World Health Organization, Laval University and Johns Hopkins University. It is meant to be used as a demonstration and decision support tool for analysts in low- and middle-income countries to examine the potential impact and cost-effectiveness of HPV vaccination. The Excel-based code with accompanying documentation is freely available online. The tool was expanded to allow multiple cohorts – it was coded in R and capability for sensitivity analysis was added, so that it could be used to automatically generate results for Gavi impact assessments.
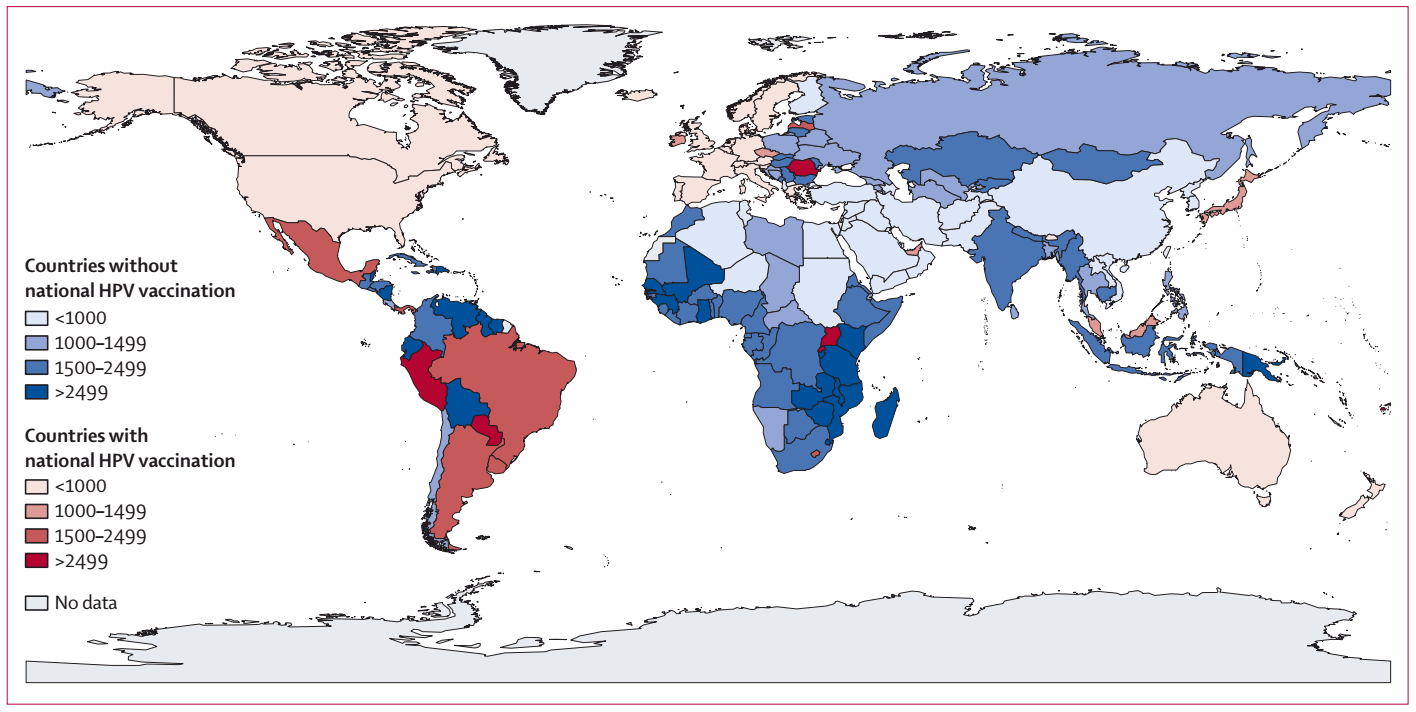
Estimated number of cervical cancers prevented per 100,000 girls vaccinated against HPV in different countries according to PRIME.
From Abbas KM, van Zandvoort K, Brisson M, Jit M. Effects of updated demography, disability weights, and cervical cancer burden on estimates of human papillomavirus vaccination impact at the global, regional, and national levels: a PRIME modelling study. The Lancet Global Health, 2020;
From Jit M, Brisson M, Portnoy A, Hutubessy R. Cost-effectiveness of female human papillomavirus vaccination in 179 countries: a PRIME modelling study. Lancet Glob Health 2014; 2(7):e406-14 Licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives License
Model name: HPV model
Modellers: Jane Kim, Allison Portnoy, Stephen Resch, Steven Sweet
Institution: Harvard School of Public Health
This companion population-based model is developed to be a simple tool to project the main features of the potential impact of HPV vaccines at the population level in settings where data are very limited. The model is constructed as a static cohort simulation model based on a structure similar to a simple decision tree, and is now programmed in R, having been previously programmed using Microsoft Excel and Visual Basic for Applications. The model tracks a cohort of girls at a target age for their lifetimes, comparing health and cost outcomes with and without HPV vaccination programs.
Unlike the more complex empirically-calibrated micro-simulation model, the companion model does not fully simulate the natural history of HPV infection and cervical cancer. Instead, the model estimates reduction in cervical cancer risk at different ages, based on several simplifying assumptions. These assumptions relate to the duration and stage distribution of, and mortality from, cervical cancer. In turn, this relies on insights from analyses performed with the micro-simulation model, using the best available data on local age-specific incidence of cervical cancer and HPV 16/18 type distribution, and assumed vaccine efficacy and vaccine coverage.
Goldie SJ1, O’Shea M, Campos NG, Diaz M, Sweet S, Kim SY. Health and economic outcomes of HPV 16,18 vaccination in 72 GAVI-eligible countries. Vaccine Volume 26, Issue 32, 29 July 2008, Pages 4080-4093
More about human papilloma virus (HPV)
Relevant publications